Patients with autoimmune disorders often suffer from severe symptoms but may find littler relief from conventional treatments. Most medications that are designed to treat these types of diseases have side effects, some of which can be severe. Understanding the drug you are taking and its effects is crucial, as is knowing the alternatives that exist. If you are taking Humira for an autoimmune disorder, you should know what your drug does, as well as the other therapies and treatments could help with your condition.
What is Humira?
Humira is a pharmaceutical manufactured by AbbVie Inc. Its scientific or generic name is adalimumab, and it is an immunosuppressive drug that is used to treat a variety of diseases, including Crohn’s disease, ulcerative colitis, chronic plaque psoriasis, rheumatoid arthritis, and other conditions. It is used to treat these diseases because it can relieve pain and reduce inflammation, especially in people with autoimmune diseases.
Humira is what is known as a biologic drug. That means it is made from cells from living organisms. This drug is genetically engineered to target specific cells in the body that are responsible for the inflammatory response. They have been found to be quite effective at treating autoimmune disorders because they target the specific components of the body that control inflammation, so they work at the source of the problem rather than mask symptoms.
Humira is sold under several names and products, including the Humira Pen, Humira Pen Psoriasis-Uveitis, Humira Pediatric Crohn’s Start, Humira Pen Crohn’s-UC-HS Start, and Humira. Patients usually administer this drug to themselves at home with a pen-like device that has a syringe to inject the medication. It must be injected, as taking it orally would destroy the active compounds in the digestive system.
How Does Humira Work?
Researchers are still learning what causes autoimmune disorders to be triggered. When you have this type of disease, your body perceives a threat that is not really there and responds as it would to disease. We have learned that TNFα, which stands for tumor necrosis factor-alpha, plays a significant role in triggering inflammation, a typical response to these threats.
Humira contains synthesized versions of a TNF blocker, which binds to the compounds that are causing the inflammatory response and effectively shut it down, reducing the pain, inflammation, and other symptoms of some autoimmune disorders (1). This medication was initially designed to treat rheumatoid arthritis, a debilitating autoimmune disease, and the name actually stands for Human Monoclonal Antibody In Rheumatoid Arthritis.
Unlike other drugs that are used to treat these autoimmune diseases, Humira targets and stops the source of the inflammation, which can lead to improved quality of life, fewer symptoms, and greater long-term outcomes for some patients. Humira is currently prescribed and recommended for the treatment of active ankylosing spondylitis, moderate to severe chronic plaque psoriasis, moderate to severe psoriatic arthritis, Crohn’s disease, juvenile idiopathic arthritis, rheumatoid arthritis, hidradenitis suppurativa, and non-infectious uveitis.
Side Effects of Humira
All medications come with some side effects, and biologics like Humira are known to have some more serious ones. The role of the active compounds in Humira is to suppress the immune system, which means that you are more prone to infections when you are taking it. Another serious consequence is that a link has been uncovered between TNF blockers and certain types of cancer, including some rare versions of the disease.
The most common side effects you make experience while taking Humira, including (2):
- Problems at the injection site, including bruising, swelling, redness, itching, and rash
- Headaches
- Nausea
- Infections, particularly in the sinuses and upper respiratory system
In addition to these minor side effects, more severe reactions may occur. You could develop a more severe infection from a fungus, bacteria, or virus, including tuberculosis. If you are carrier of Hepatitis B, you can develop an infection, as well. Some people experience allergic reactions to the medication, which can result in wheezing, difficulty breathing, chest tightness, hives, rash, itching, and swelling in the face, lips, or tongue.
Humira can cause problems in the nervous system, including dizziness, vision problems, or trouble in extremities, including numbness, tingling, and weakness. Your doctor may not recommend Humira if you have multiple sclerosis or Guillain-Barré syndrome. This medication can lead to or worsen heart problems, causing swelling in the extremities, shortness of breath, and sudden weight gain.
Your immune system may respond to this medication and react with symptoms that resemble Lupus. These can include rash, joint pain, shortness of breath, and chest pain. Other side effects include blood problems such as bruising or low red blood cell count and liver troubles.
Interactions
For those who are allergic to adalimumab or the compounds in this medication, you should not take Humira. Those with an infection should not start using Humira, so you should share with your doctor if you have cough, fatigue, aches, chills, fever, skin sores, digestive problems, or any other symptom that could be from an infection.
There are several medications that should not be taken with Humira. Always tell your doctor about any medications, supplements, or herbs you take, including those you start taking after you begin using Humira.
Among those to be most cautious about, the following drugs may interact with this medication (3):
- Abatacept (Orencia) or etanercept (Enbrel)
- Anakinra (Kineret)
- Azathioprine (AZA) or mercaptopurine (6-MP)
- Certolizumab (Cimzia), golimumab (Simponi), infliximab (Remicade), or rituximab (RITUXAN)
Certain medical conditions can interact with Humira.
You should talk with your doctor about any of the following conditions or symptoms before starting this medication.
- Tuberculosis, including if others in your house have this disease
- Diabetes
- Cancer
- Hepatitis B
- Congestive Heart Failure
Humira may cause problems for those with a latex allergy and is not recommended if you are scheduled for surgery. If you have recently had a vaccine or plan to get one soon, talk to your doctor. You should not take Humira while getting any live vaccine, which includes those for yellow fever, measles-mumps-rubella (MMR), varicella, shingles, or the flu-mist vaccine.
Humira is not recommended for young children, women who are pregnant or breastfeeding, or those who plan to travel outside the U.S.
Alternatives to Humira
There are other medications and therapies that are available to treat the diseases that Humira is prescribed for, as well. For example, for the treatment of rheumatoid arthritis or Crohn’s disease, other biologics have been developed, including Cimzia, Enbrel, Remicade, and Simponi. Below, we explain the alternative for the most common illnesses that Humira can treat.
Because Humira is made from living material, it is difficult to duplicate, which is why no generic form of the drug is on the horizon in the near future. However, there are two biosimilar drugs, Amjevita and Cyltezo, which have been approved by the FDA and are in clinical testing.
These are not yet available to the public, though.
Alternatives for Treating Crohn’s Disease
The goal of any treatment for Crohn’s disease is to reduce inflammation, relieve the pain and diarrhea associated with the disease, and address any nutritional deficiencies that result from the digestive disorder. Most commonly, this treatment involves prescription medications or surgery combined with other therapies.
Treatment options will depend on the severity and nature of your disease. Other than Humira, drugs used to treat Crohn’s include those designed to reduce inflammation, including sulfasalazine and other 5-amino salicylic acid (5-ASA) medications.
Sometimes, patients are given corticosteroids to reduce inflammation, as well. This is usually to minimize initial inflammation, and these are reduced once other treatments have begun. Other types of immunosuppressants can also be used to reduce the inflammatory response. Other biologics that block different inflammatory markers are being introduced, as well, including Tysabri and Entyvio.
Those with Crohn’s may also use nutritional supplements to address any deficiencies that result from their disease (4).
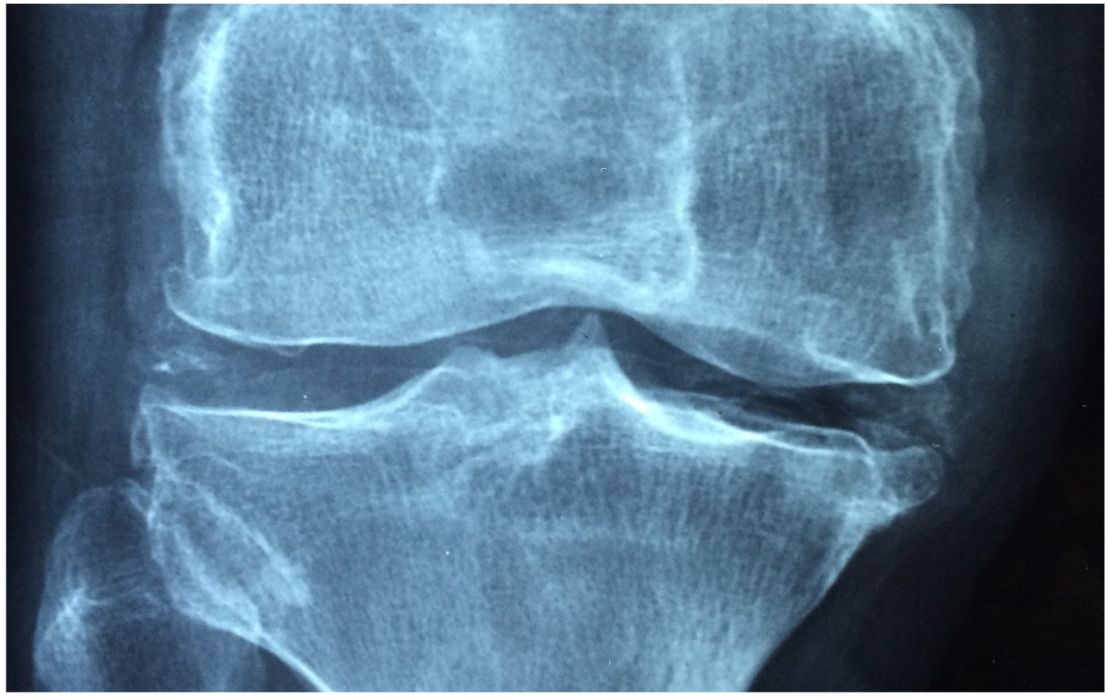
Alternatives for Treating Rheumatoid Arthritis
There are many different options for treating rheumatoid arthritis (RA). Medications are designed to address the pain and inflammation of the disease. Others may reduce the damage caused by this condition. Common medicines for RA that are available over the counter include nonsteroidal anti-inflammatory drugs (NSAIDs, corticosteroids, and acetaminophen. Prescriptions that are commonly used to treat this disease include (5):
- Disease-modifying antirheumatic drugs (DMARDs)
- Janus kinase (JAK) inhibitors
Many people respond well to other forms of therapy for RA, including using exercise, rest, heat, or cold to relieve symptoms. Some wear assistive devices that hold their joints in a specific resting condition, which can lower inflammation. Other devices may help you to move and complete daily tasks when the range of motion is limited.
Alternative for Treating Plaque Psoriasis
Treating plaque psoriasis is like other autoimmune diseases in that treatments are designed to limit the symptoms, but there is no known cure for the disease. If you want an alternative to Humira to treat your moderate to severe plaque psoriasis, your options are somewhat limited. Some patients respond well to light therapy, where your skin is exposed to ultraviolet light. Most people with more severe forms of the disease require a treatment that targets the immune system.
These medications calm the inflammatory response and can cause excess skin cells to grow more slowly.Common options of this kind include acitretin, cyclosporine, and methotrexate, which can be taken orally or given as a shot (6). Other biologics that are used to treat plaque psoriasis include infliximab (Remicade), brodalumab (Siliq), etanercept (Enbrel), secukinumab (Cosentyx), guselkumab (Tremfya), risankisumab-rzaa (SKYRIZI)), ixekizumab (Taltz), and ustekinumab (Stelara).
Many of these have similar side effects to Humira.
PEMF Therapy as an Alternative to Humira
Some people may choose to forgo medication altogether and seek alternative therapies for their autoimmune disorder. For those with rheumatoid arthritis, Crohn’s disease, and other conditions resulting from an overactive inflammatory response, pulsed electromagnetic field (PEMF) therapy presents a viable alternative. PEMF therapy is the use of low-frequency, low-intensity pulses of electromagnetic energy to stimulate cellular function and repair. A device emits these pulses of energy, which can be directed at specific locations or used more diffusely.
The electromagnetic waves restore the cell’s natural energy levels, which enables them to work more effectively and perform their necessary functions. Your body releases T cells within the immune system, which are the controllers of the inflammatory response.
This reaction is generally designed to protect the body from harm, but when these cells are overactive, they can cause long-term damage and result in pain and inflammation that becomes chronic. PEMF controls inflammation by deactivating these T cells, thus shutting down inflammation in targeted areas.
PEMF therapy has been shown to help control inflammation in many different conditions, including rheumatoid arthritis, osteoarthritis, tendinitis, fibromyalgia, and other autoimmune disorders. It is a well-respected therapy for the use in the treatment of these diseases, and because it has no adverse side effects, it also is well tolerated by more people.
In addition to controlling the pain and inflammation of rheumatoid arthritis, PEMF therapy can also help improve the underlying structure of the bone, which becomes damaged over time from this disease. Research studies have documents PEMF therapy’s ability to reduce cartilage damage and deterioration due to RA while also preserving bone tissue.
While reducing inflammation, PEMF therapy can also improve the circulation of nutrients and oxygen to inflamed joints and tissues. Those with fibromyalgia, Crohn’s disease, and other chronic disorders that result from an overactive inflammatory response can benefit from this therapy with fewer symptoms, improved cell structure and function, and overall improvement in their health.
Final Thoughts
Humira is a biologic medication that is manufactured from living cells. It blocks the TNFα that is known to cause the inflammatory response. Humira is prescribed to those with ankylosing spondylitis, plaque psoriasis, psoriatic arthritis, Crohn’s disease, juvenile idiopathic arthritis, rheumatoid arthritis, hidradenitis suppurativa, and non-infectious uveitis.
While this medication can be effective for some, it has serious risks, side effects, and interactions that should be considered before taking it. For those looking for alternatives to Humira, there are many other conventional treatments available.
PEMF therapy is also an excellent choice for the treatment of many inflammatory conditions, including rheumatoid arthritis, psoriasis, and Crohn’s disease.